Diabetic Retinopathy
Diabetic Retinopathy
The increased prevalence of diabetes is gaining a great concern worldwide. Diabetic retinopathy (DR) is the most common cause of blindness in people under the age of 65. Insulin resistance and prolonged hyperglycemia are of the main reasons behind blood retinal barrier dysfunction and diabetic retinal damage. Neurodegeneration is a crucial factor in early diabetic retinopathy. Diabetic retinopathy harms the optic nerve by producing damage to its integrity and conductivity.
Signaling Pathways:
Chronic diabetes leads to the activation of a number of signaling proteins that contributes to diabetic retinopathy including protein kinase C, protein kinase B, and mitogen-activated protein kinases. These signaling cascades are activated in response to hyperglycemia-induced oxidative stress, polyol pathway, and advanced glycation end product formation. The aberrant signaling pathways ultimately lead to activation of transcription factors such as nuclear factor-kappaB and activating protein-1.
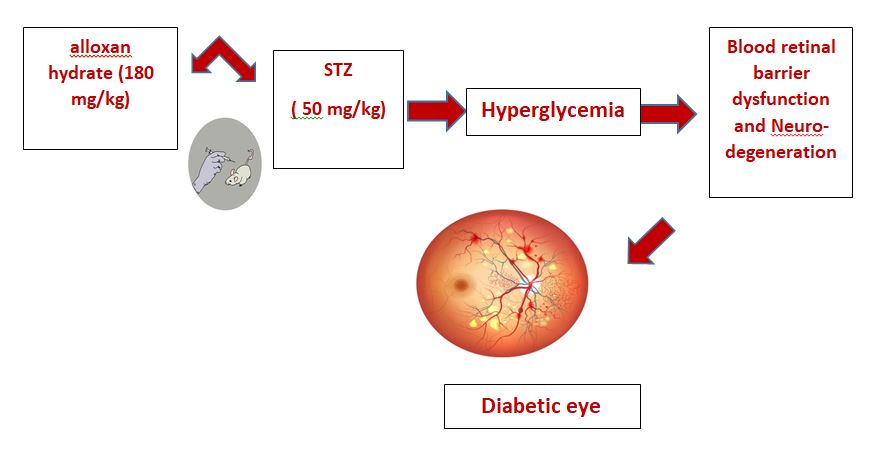
Induction of diabetic retinopathy:
- Type 1 diabetes mellitus is prompted through one subcutaneous injection of alloxan hydrate (180 mg/kg). Mice are counted diabetic when the glucose level in blood is >250 mg/dl 1 week after injection of alloxan.
- Rats are injected intraperitoneally (IP) with streptozotocin (STZ) at 50 mg/kg to induce diabetes. Mice are injected with STZ for three consecutive days, while rats receive a single IP dose (animals are fasted for 4 h prior to injection). The mice and rats are evaluated 3 days after the STZ injection series to determine if they are sufficiently diabetic. A blood glucose concentration that exceeds 300 mg/dL is considered diabetic.